Balancing Blood Sugar: The Key to Hormonal Harmony
Article contributed by Courtney van der Scheer from Reframe Nutrition.
In the world of health and wellness, “balancing blood sugar” is a term that’s often mentioned, especially if you have any symptoms such as infertility, energy crashes, brain fog, or stubborn weight gain.
But do we know why “balancing blood sugars” is necessary? Why do we even care about the sugar that’s in our blood and what it’s doing? Today, we’re going to answer those questions, and more. Because maintaining stable blood sugar is foundational to overall health, it plays a pivotal role in energy, mood, weight, and the delicate balance of the body's systems. We’ll dive into the role of insulin, examining how its dominance impacts other key functions and how you can easily monitor your blood sugars, in real time using a CGM (continuous glucose monitor). We'll also touch on Dr. Mindy Pelz’s hierarchy of hormones, highlighting how blood sugar management underpins optimal hormonal health.

Blood Sugar Basics: What Happens When It's Out of Balance?
Blood sugar, or glucose, is the primary fuel for our cells. It comes from the carbohydrates in food, converted into glucose during digestion. Remember, though, that we don’t need a lot of breads and pastas to obtain glucose. Things like vegetables can have sufficient glucose in them for our cells…. What I’m trying to say here, is that we don’t need to eat the 9 servings of breads and pastas per day to get the glucose our bodies need. If you’re a high performance athlete, that’s a different story. I’m talking to the average middle-aged person here.
The body has a finely tuned system to maintain glucose levels within a narrow range, ensuring the brain and muscles have a steady energy supply. However, frequent spikes and crashes in blood sugar—caused by diets high in refined carbs and sugar—can wreak havoc. Here’s what can happen:
- Energy rollercoasters: High blood sugar gives a quick energy boost, but it’s often followed by a crash, leaving you fatigued and craving more sugar.
- Weight gain: Excess glucose is stored in the liver, muscle and then in fat cells. And if we don’t have enough fat cells, our body will lay down more in order to store that glucose. This is particularly true for the abdomen.
- Inflammation: Chronic blood sugar spikes can lead to systemic inflammation, a precursor to many chronic diseases. When blood sugar is high your immune system jumps into action. Inflammatory molecules, such as white blood cells and cytokines, work to break down the glucose. As a result, inflammation occurs.
- Hormonal imbalances: High blood sugar triggers insulin, a key hormone that can overshadow others, disrupting your hormonal balance (more below).
Insulin: The Master Regulator
Insulin is a hormone produced by the pancreas, essential for regulating blood sugar. After you eat, your blood sugar rises, prompting insulin to shuttle glucose into cells for energy or storage. Think of insulin as a "key" that unlocks cells to let glucose in. The body views excess blood sugar as a threat. Elevated blood sugar is toxic to tissues and organs, so managing it is a top priority. When blood sugar levels rise, insulin takes centre stage, temporarily putting other processes—like fat-burning and other hormone production—on hold. Basically, our bodies prioritise insulin over many other hormones. Insulin is like a little bully, fighting off oestrogen or progesterone (as an example) on the cell, for it's more important job of putting away glucose(c).
The Hormonal Domino Effect: Insulin’s Priority Disrupts Balance
Hormones work in a finely tuned system, communicating to maintain homeostasis. However, when insulin becomes the focus, it can disrupt this balance. Here’s how it happens:
- Cortisol (Stress hormone)
Blood sugar instability often triggers cortisol, the stress hormone, to prevent dangerous dips in blood sugar. Chronic cortisol elevation can lead to adrenal fatigue and worsen insulin resistance. - Thyroid hormones
Insulin resistance interferes with thyroid function, slowing metabolism. The body prioritises blood sugar regulation over thyroid health, often leading to symptoms like fatigue and weight gain (d) - Sex hormones (estrogen, progesterone, testosterone)
Insulin resistance impacts ovaries and testes, disrupting hormone production. This imbalance can cause irregular cycles, PMS, or low libido. And is why you’ll often hear ‘insulin resistance’ being linked to poly-cystic ovarian syndrome, a hormonal dysfunction that can lead to infertility. - Leptin (hunger hormone)
Elevated insulin can lead to leptin resistance, where the brain no longer receives signals that you’re full, driving overeating.
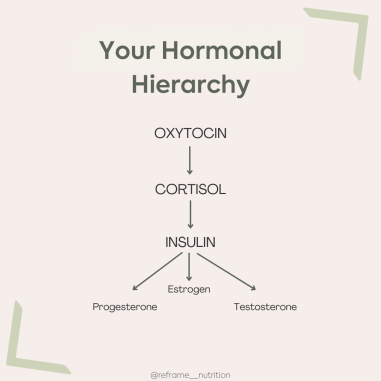
Hierarchy of Hormones
Dr. Mindy Pelz, a leading expert in women’s health and fasting, emphasises that hormones voperate in a hierarchy. According to her (and many others), the body prioritises certain hormones over others, much like Maslow’s hierarchy of needs. Here’s the order:
- Survival hormones (oxytocin – cortisol – insulin)
These are vital for immediate survival. Oxytocin is at the top of the food chain, he promotes bonding and will calm cortisol. Cortisol spikes will cause increases in insulin and insulin surges have a direct effect on your sex hormones. - Sex Hormones (estrogen, progesterone, testosterone)
Reproductive health is the final priority. If survival is compromised, sex hormone production takes a backseat.
In this framework, insulin’s dominance is clear: if blood sugar isn’t stable, it’s nearly impossible for the body to optimise reproductive or thyroid hormones(a). Thyroid hormones fit in before the sex hormones as they’re involved with metabolism. But I left that out here for simplicity. The fundamentals are – you can’t balance your sex hormones if you haven’t got your cortisol or insulin under control.
Why Do We Care? The Long-Term Impacts of Poor Blood Sugar Control
Chronic blood sugar imbalances contribute to a range of health issues, including:
- Type 2 diabetes: Persistent insulin resistance can overwhelm the pancreas, leading to diabetes.
- Heart disease: High insulin levels promote inflammation and fat storage, increasing cardiovascular risk.
- Hormonal disorders: Conditions like PCOS, infertility, and thyroid dysfunction are closely linked to insulin dysregulation.
- Cognitive decline: High blood sugar and insulin resistance are associated with Alzheimer’s, often called "type 3 diabetes”(b).
Steps to Balance Blood Sugar
Balancing blood sugar isn’t complicated, but it does require consistent habits. Here’s how:
- Prioritise protein and healthy fats
These macronutrients slow glucose absorption, keeping blood sugar stable. - Eat fibre-rich foods
Fibre reduces the speed at which glucose enters the bloodstream. - Savoury breakfast
Avoid sugar-laden breakfast cereals or toast with honey/jam. This sets you up for a rollercoaster of blood sugar spikes from the get-go. - Strength or resistance training
Muscle is a reservoir for glucose, by increasing muscle mass, you increase the area for glucose storage. - Manage Stress
High cortisol from chronic stress worsens blood sugar spikes. Incorporate stress- reducing practices like meditation or yoga. - Sleep Well
Poor sleep elevates cortisol and disrupts insulin regulation.
Where does a Continuous Glucose Monitor (CGM) fit in?
A Continous Glucose Monitor (CGM) is a tiny device worn on the tricip or abdomen, capable of sending real time glucose data to your phone via bluetooth. Modern devices like LinX CGM from ReadyMode last as long as 15-days and allow you to view the trends, peaks and troughs of your glucose levels during the day and even overnight when you sleep. The also allow the user to export detailed reports for more in depth analysis.
This technology was originally designed to help people with diabetes make dosing decisions without relying on fingerpricks and avoid dangerous states of low or high blood glucose. However, as CGMs are becoming more widely available, their value is increasingly being recognised as a tool to gain metabolic insights and help individuals make heathier choices, even for those who do not have prediabetes or diabetes. Prevention is better than cure and we’ve already discussed the reasons why managing blood sugars is key to long-term health.
We are all individuals. What white rice does to me, won’t necessarily be the same for you. By using a CGM, we can get very specific in tuning your individual nutrition programme and really find out what truly works for you and what does not. Also, seeing the impact of your breakfast, or that cheeky caramel latte, on your glucose levels in real time, might just push you to kick off some changes that you've been putting off for a while. I've observed this to be especially true for some of my clients living with type 2 diabetes or prediabetes where “out of sight, out of mind” has played a role on their lifestyle choices - adding real real time CGM insights can be a powerful motivator for change. I’m very passionate about supporting people to improve their health-span and health outcomes, so this really excites me!
If you’re confident you've already got positive lifestyle habits in place, wearing a CGM can still help support this further – for example a client of mine is an avid hiker. When she wore a CGM, we found her blood glucose was dropping quite significantly overnight, so we tweaked her diet to include more fuel after days out hiking. This immediately improved her recovery and sleep quality and she wasn’t so fatigued the next day. I’ve personally begun using CGM recently and it's led to some really great insights. There are more details on my Instagram page, but I noticed the impact of sleep on my blood sugars, and that by having fat and protein with my carbohydrates, my blood glucose levels didn't get nearly as high after eating. I get my sensors from a local NZ company, based here in the Waikato, ReadyMode.
Conclusion
Balancing blood sugar isn’t just about avoiding energy crashes—it’s foundational for overall health. By prioritising stable blood sugar, you give your body the tools it needs to regulate other hormones, reduce inflammation, and prevent chronic disease. When insulin takes centre stage, other hormones take a backseat, leading to a cascade of imbalances. By understanding the hormonal hierarchy and adopting lifestyle changes that support blood sugar stability, you can restore homeostasis to your body and give yourself a better chance at long term vitality and increased health-span; what do you need to do today to be the 80-year-old you want to be?
About the Author
Courtney van der Scheer is a Registered Clinical Nutritionist and founder of Reframe Nutrition. Courtney is passionate about hormonal health and solving complex issues, specifically for women during perimenopause and beyond. She uses a multi-faceted, holistic approach to support her clients and offers consults via video link or in -person in the Waikato. You can read more about Courtney and her personal journey with health and nutrition here or follow her on instagram or facebook.
References:
(a) Pelz, M. (2021). Fasting Like a Girl: A Woman's Guide to Using the Power of Fasting to Lose Weight, Balance Hormones, and Boost Energy. Lioncrest Publishing.
(b) Nguyen TT, Ta QTH, Nguyen TKO, Nguyen TTD, Giau VV. Type 3 Diabetes and Its Role Implications in Alzheimer's Disease. Int J Mol Sci. 2020;21(9):3165. Published 2020 Apr 30. doi:10.3390/ijms21093165
(c) Peppa, M., Koliaki, C., Nikolopoulos, P. & Raptis, S. A. Skeletal muscle insulin resistance in endocrine disease. J. Biomed. Biotechnol. 2010, 527850–527850 (2010).
(d) Kocatürk E, Kar E, Küskü Kiraz Z, Alataş Ö. Insulin resistance and pancreatic β cell dysfunction are associated with thyroid hormone functions: A cross-sectional hospital-based study in Turkey. Diabetes Metab Syndr Clin Res Rev. 2020;14(6):2147-2151. doi:10.1016/j.dsx.2020.11.008.